John Pilger’s latest film, Utopia, recently aired on SBS television. New Matilda owner/editor Chris Graham worked as an associate producer on the film. In this special feature, he provides an inside look at the making of Utopia.
SPECIAL REPORT: Sometimes in life, you can feel pretty helpless. That said, I’m a privileged white guy in a privileged white society. So for me at least, it doesn’t happen very often.
It happened last year.
At the time, I was the managing editor of Tracker magazine. The NSW Aboriginal Land Council, owner of Tracker, was generous enough to give me time to fulfill a childhood dream.
John Pilger is a journalist I grew up reading, and a largepart of the reason why I entered journalism.
Pilger was back in Australia making his fourth film about the plight of Aboriginal Australians.
He asked me to work on it with him. I didn’t feel helpless, but I certainly felt daunted. The helplessness was to come.

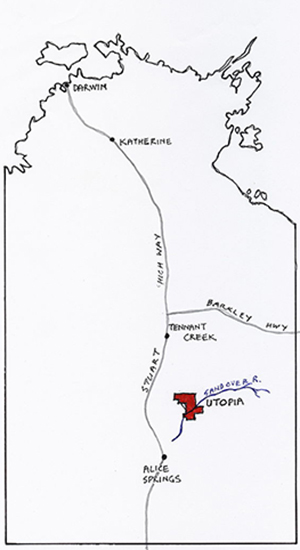
One of the first major shoots was in Central Australia, and we spent the better part of a week filming in and around Ampilatwatja (pronounced Um-budder-watch), a small Aboriginal community 300 kilometres north east of Alice Springs on the edge of a vast region known as Utopia.
Most disadvantaged
I’d been to Ampilatwatja many times before. Previously I had written a news feature about research out of the Centre for Aboriginal Economic Policy Research (CAEPR), which had ranked the region as the most disadvantaged in the nation.
Strangely, only a few years earlier, the Menzies School of Health Research had also noted in a study that despite its poverty, Utopia also had a mortality rate around 50 percent lower than the rest of the Northern Territory.
That makes Utopia a very unique place – despite its grinding poverty, its people live longer than many of their countrymen throughout the Territory, due in large part to the fact Aboriginal people in the region still live a semi-traditional lifestyle.
Governance structures are largely in place, and people stave off their hunger with a semi-traditional diet.
So the trip to Ampilatwatja with Pilger, co-director Alan Lowery and his crew would provide some familiar surrounds.
During the shoot, John, Alan and I stayed in the nurses’ quarters – modest staff housing across the road from the Ampilatwatja Health Clinic.
Preston Clothier (director of photography) and his crew stayed in the doctor’s house opposite.
Long, hot day
After a full day of shooting – including a trip to a remote outstation to film David Smith, CEO of the Health Service at work – we all met back at the nurses’ quarters for dinner.
 It had been a long, hot day – Utopia in Spring feels like the worst of a stifling Sydney summer day, and the dry heat takes it out of you. Most of the crew and half of the health clinic staff didn’t last until 8pm, before retiring for bed.
It had been a long, hot day – Utopia in Spring feels like the worst of a stifling Sydney summer day, and the dry heat takes it out of you. Most of the crew and half of the health clinic staff didn’t last until 8pm, before retiring for bed.
John snuck off to his room to do some research (standard practice, I was to discover) while Alan, myself and two of the clinic’s nurses, Jackie and Margaret, stayed up to chat.
Shortly after 9pm, our conversation was interrupted with a loud banging on the front door.
Jackie was on call, so she went to answer.
A frantic young Aboriginal woman was on the steps, and she pleaded with Jackie for help.
Margaret, although not on call, rushed out the door with her.
Alert, not alarmed
Alan and I stayed. We figured someone – probably a kid – had injured themselves. Broken an arm, trod on a nail, fell off her bike, as kids often do. To quote John Howard, we were alert, but not alarmed.
A short time later, there was more loud banging at the door. I went to answer it. Now, two men were outside. Both seemed very frightened, and suddenly, I was the one fielding the pleas for help.
“They want you to come. They need your help,” one of the men said.
I know nothing about medicine. Beyond lifting something for someone, I couldn’t imagine what help I could possibly provide.
“Are you sure they want me,” I asked.
“Yes, they want you. You have to come.”
“Are you sure it’s me?”
‘They want you’
“Yes, yes, you. They want you.”
“Where are they?” I asked.
“In the camp. Behind the clinic. They need you, quick.”
“I’m coming,” I replied.
I rushed back inside and grabbed my shoes. Alan agreed to hold the fort. I headed out the door.
The drive was only a few hundred metres – I could have run there quicker – and when I arrived, the men who’d come to the house waved me off the road into a paddock adjoining the health clinic.
It was immediately apparent to me that I wasn’t the person that Jackie and Margaret – the nurses – had sent the men to find. They wanted the local doctor, Laura, not a visiting journalist.
Tin humpy
The area immediately around a small tin humpy bordering the health clinic was lit up with spotlights from the Ampilatwatja bush ambulance.
Jackie, Margaret and Dave Smith were performing CPR on a figured slumped in the humpy.
As I arrived, they started loading the body of a man into the back of the ambulance. Jackie was pumping away furiously on the man’s chest as they did.
CPR on television always looks quite clinical and controlled. In the real world, it’s a pretty violent process. And it’s hard to watch, particularly if you know anything about CPR. Because when things have reached that point, statistically speaking the outcome is often bad.
Dave wheeled the 4WD around, drove past me, wound his window down and yelled, ‘Clinic’.
“Yep,” I replied, and followed him the 25 metres or so back to the front door.
By the time the ambulance pulled up, the men and women from the humpy camp were already milling around the emergency entrance.
Pumping his chest
Jackie, Margaret and Dave rushed the man into the building, pumping on his chest as they went, and forcing oxygen into his lungs via a bottle and mask.
I followed, my head spinning.
As I entered, Jackie was still pumping away on his chest. Margaret was still administering oxygen. Dave was rushing around preparing a cart, which I guessed was a defibrillator.
“What can I do?’ I asked Dave. “Do you want me to get the doctor?”
“Yep, that’d help. Thanks.”
I ran the 50 metres back up the road to the doctor’s residence, and banged on the front door.
One of the film crew was the first to wake. I told him Laura was needed urgently. He went to wake her, and I ran back to the clinic.
Clinic gurney
As I entered the room, Dave, Margaret and Jackie were still working on the man. They were lifting him from the ambulance bed onto a clinic gurney.
He crashed down on to the bed, and Dave took over the CPR, barely skipping a beat.
Margaret was straight back on to the oxygen. Jackie was now preparing machines.
It was an extraordinary thing to witness. And chilling.
Dave pushed the ambulance bed towards me. “Get this out of the way,” he snapped.
I moved it a few feet further towards the door, the sum total of my assistance so far, and a clear pointer to the reality that my presence was absolutely, utterly irrelevant.
Like a voyeur
On the one hand, I didn’t want to leave. It felt like I would have been running from a bad situation. But I didn’t want to stay either. I felt like a voyeur, like I was seeing something I shouldn’t. So I walked outside and leant against the ambulance.
I think some of the men outside were wondering why the ‘doctor’ – sitting on the back step of the ambulance looking stunned – wasn’t in working on their friend.
One of the men approached. “You alright?” I said.
“Yeah.”
“What happened?” I asked.
“Don’t know. He was workin’ today. He was all good. Then he just crashed.”
Laura and her husband Justin, also a nurse at the clinic, arrived and rushed into the clinic.
Commotion inside
We could all hear the commotion inside. And then after a minute or two, it just stopped.
Dave Smith emerged a few minutes later.
“Whose this man’s brother’s uncle?”
There was no response from the group.
“Whose this man’s brother’s uncle?” Dave repeated.
Again, no response.
“Who is responsible for this man? Who speaks for this man?”
Some of the men pointed to an old man standing just to Dave’s left.
Old man’s hand
Dave turned, extended his arm and shook the old man’s hand.
“I’m sorry. You saw where we were working. You saw what we were doing. We did everything we could. You saw it. You saw how hard we worked. We tried. We worked hard on that man. But we couldn’t do anything. It was up to God. I’m sorry. We did all we could. But it was up to God.”
And then that was it.
The men each thanked Dave by shaking his hand, then turned and walked away.
As they did, a woman who’d been watching from the shadows rushed forward. The enormity of the news Dave had just delivered had obviously dawned on her, and she collapsed in the dirt, wailing.
It was the woman who’d come to the door to get the nurses. She was the man’s partner.
His name was Mr Davey. He was 47 years of age.
Appeared from shadows
Several more women who I hadn’t noticed appeared from the shadows and lifted the woman from the ground, comforting her.
They too started wailing.
The sound of Aboriginal women mourning a death is hard to describe, save to say it cuts right through you.
I stood frozen, unable to speak, too ashamed to cry.
The men and women started to walk north down the main community road. The wailing intensified as they did, as more and more people learned the tragic news.
It lasted much of the night.
I walked back into the clinic with Dave, my sense of utter helplessness now complete.
All I wanted to do was disappear.
Lifeless body
As a last act of impotence, I made the staff tea and coffee, then excused myself.
My last memory of the clinic is Mr Davey’s lifeless body lying on a bed, alone in the corner.
When I made it back to the house, Alan was still up, waiting. I must have looked a little shell-shocked.
“Not a good outcome, I take it?” said Alan.
“Yeah. Not good,” I replied.
“I heard the wailing.”
“Yeah, a man just died.”
Nurses returned
The nurses returned home a few hours later. None of us got much sleep.
We woke early the next morning. The humpy in which Mr Davey lived was already gone – the community had already cleaned up the site.
It was like the whole thing had never happened, that it was just a very bad dream.
In most Aboriginal communities, when an Aboriginal person dies inside a house, the whole family must move out. With a humpy, it’s much easier – they just pull it apart. As Pilger notes in Utopia, when an Aboriginal person in Central Australia dies, their house dies with them.
Dave Smith was also up early, although he looked like he hadn’t slept at all.
His comments to the men – that they had seen how hard he and his staff had worked – had confused me.
I asked him why he’d phrased it that way, as though he was trying to deflect blame for what clearly seemed to be a blameless death.
Unexplained death
Dave explained said that in Central Australian Aboriginal communities, you can’t have an unexplained death.
Children and old people die – to the Alyawarra people, that’s explainable, understandable. But the death of a seemingly healthy, middle-aged man needed to be explained. And someone had to be held responsible.
Dave was concerned his staff would be the ‘someone’.
Of course, Mr Davey’s death was entirely explainable. Finding who’s responsible is a little trickier, but I’ll come to that.
Mr Davey died of a heart attack. The most likely cause was rheumatic heart disease, something he’d probably contracted many, many years earlier.
Like trachoma, rheumatic heart disease is a third-world condition which has been all but eliminated from Western countries.
With one exception.
Rheumatic heart disease
Aboriginal people in remote regions of Australia – particularly Central Australia – have the highest recorded rates of rheumatic heart disease on earth.
It’s an entirely preventable disease caused, primarily, by poor living conditions and overcrowding.
The Utopia region is a beautiful place, with beautiful people. But poor living conditions and overcrowding are rife.
Families in Ampilatwatja routinely cram more than a dozen people into a single dwelling, sometimes as many as 30.
On top of that, dozens more sleep in backyards on old wooden doors or bed bases propped up by overturned paint tins.
The single men’s quarters in Ampilatwatja is tiny – an old tin shed with no running water, and no electricity. It has holes in the walls and is barely fit to store tools. But it’s routinely home to more than half a dozen men.
Eric Elkedra, a local Aboriginal health worker who is interviewed by Pilger in Utopia, also lives in a tin shed with his wife and two kids.
Holes in wall
It has also holes in the walls, no running water, no electricity. Despite this, the federal government collects rent from him every fortnight.
And those that aren’t lucky enough to have a permanent dwelling – like Mr Davey – sleep in humpies on the edge of the community. A humpy is a simple wood structure. Sometimes shade is provided by tin, sometimes by tree branches.
Meanwhile a ‘Government Business Manager’ appointed as part of the Northern Territory intervention lives in a sprawling compound with multiple rooms and more than a dozen air-conditioners.
Just a few years ago, the population of Ampilatwatja abandoned their community and set up camp in the bush after raw sewage had been pooling in the streets for months.
The sewerage system was eventually patched up although it still breaks down regularly today.
When the NT intervention rolled into town in early 2008, no new homes were built to relieve the overcrowding, despite the expenditure across the Territory of more than $1 billion on housing.
Instead, the old Ampilatwatja homes – most of them built in the ATSIC days – got a lick of paint, and then, eventually, dodgy renovations which did precisely nothing to relieve the staggering levels of overcrowding.
New BMX track
The NT intervention also delivered a new BMX track – a grader and some white men arrived one morning to push mounds of dirt together.
A shipping container full of BMX bikes with the words ‘Ampilatwatja BMX Club’ painted on the side also arrived.
Unfortunately, the key to the container was stored hundreds of kilometres away in Alice Springs, lest the local kids think they might actually be able to access the bikes whenever they want, or get something tangible from legislation which suspended their basic human rights.
The Ampilatwatja BMX club opened its doors once, and then the shipping container sat rusting for the next few years.
Ampilatwatja, like all remote Aboriginal communities, has suffered from a long bureaucratic malaise, so while there’s an obvious collective responsibility for the conditions in which people like Mr Davey lived and died, it’s harder to sheet home individual blame.
But it’s not impossible.
Just a few hours before Mr Davey died, the Ampilatwatja Health Clinic received a surprise visit from Warren Snowdon, the federal Minister for Indigenous Health.
Snowdon also happens to be the long-serving Member for Lingiari, the federal seat which takes in most of the Northern Territory.
He’s held that position for more than two decades.
Short notice
The visit was short notice, but Snowdon stayed for several hours.
Dave Smith and his staff wanted to talk about the needs of the clinic and the needs of the community.
Snowdon, however, kept steering the conversation back to governance, and the importance of community leadership.
The irony, of course, is perverse.
As Snowdon prepared to leave, nurse Jackie decided to collar the minister as he was walking out the door.
Apart from nursing, Jackie’s other expertise is in environmental health. She wanted Snowdon to understand that the government could provide all the primary health care that one of the wealthiest nations on earth could afford, but it wouldn’t make a lick of difference if the environmental health problems weren’t also addressed.
Jackie wanted to talk about the simple things that government could do – lids for community rubbish bins. Proper sewerage systems.
Snowdon nodded politely, as though he understood.
Thousands of times
Indeed Snowdon likely did understand, because it’s a message that has no doubt been delivered to him thousands of times as the Member for Lingiari, and hundreds of times as the Minister for Indigenous Health.
And yet the atrocious environmental health conditions endure, and have done throughout Snowdon’s entire time in office as the advocate in Canberra for the dirt poor people of Ampilatwatja.
It all begs the question: why?
A few months later, Pilger got to ask exactly that question of Warren Snowdon during an interview in the decadent and advantaged surrounds of Parliament House in Canberra.
As Pilger notes in Utopia, the contrast between the grinding disadvantage of Ampilatwatja and the obscene wealth and privilege of Canberra couldn’t be more stark.
I don’t want to spoil the punch-line of Pilger’s exchange with Snowdon – you’ll have to watch the film – but let’s just say one of the things for which Pilger is best known is holding power to account, and he does that in spades with a seething, bombastic Snowdon.
I sat in on that interview, as Pilger applied the blowtorch to a nervous, gulping but increasingly defiant Snowdon.
Stark difference
Looking back, I too felt a stark difference between Canberra and Ampilatwatja, although for far more personal reasons.
In Ampilatwatja I could do nothing but stand and watch as a group of extraordinary people battled hopelessly to save the life of an Aboriginal man who had been condemned to die years earlier, a victim of political blame-shifting and official national indifference.
But in Canberra, watching Snowdon stripped bare in front a camera by one of the world’s foremost journalists – being asked the sorts of questions Snowdon should be asked every day, but never is – I was reminded that I probably wasn’t the only one who felt like they served no useful purpose in Ampilatwatja the day that Mr Davey died.
After meeting with Dave Smith and the crew from the Health Clinic, Snowdon and his staff piled back into a brand new Toyota Landcruiser to head back to Alice Springs.
And then, as if by after-thought, a Snowdon staffer emerged from the vehicle and rushed back into the clinic.
He was carrying two bags of fruit, and left them for the staff – an act of Ministerial generosity.
One of the bags was full of mouldy oranges.
This feature was first published in the soon to be defunct Tracker magazine. Utopia recently had a debut on Australian television on SBS. The article has been republished here with the permission of New Matilda.