Most of the growing numbers of women who are imprisoned in the Australian state of New South Wales are suffering psychiatric disorders. In a rare glimpse into Silverwater Corrections Centre, Inga Ting investigates and finds that imprisonment itself may be making mental health problems worse.
Jennifer*, a mother and university graduate, says she would not have considered herself at risk of suicide or self harm when she entered the Australian prison system early in 2010. Before February, when she was arrested for a crime committed more than 12 years ago, Jennifer was enjoying a successful academic career, leading a vibrant social life and flourishing in a stable, long-term relationship.
But after just six weeks in Silverwater Women’s Correctional Centre – a maximum security facility where remand detainees are housed alongside the state’s most dangerous women offenders – her self-confidence, her outlook and her life are in tatters.
“They claim the system isn’t punitive, they claim it’s supposed to help you rehabilitate,” Jennifer says. “I feel like I’ve lost ... my ability to interact with the world. I was a very confident and strong woman before all this started and I have trouble conceiving of ever getting back to that stage again ... [T]he prison system has pretty much destroyed any semblance of mental health that I had.”
Jennifer was diagnosed with borderline personality disorder, anxiety and depression in her early-20s but after eight years of psychiatric treatment learned to successfully manage these problems. Her psychiatrist, Dr Young, says her last major depressive episode prior to prison was more than five years ago. On the day she set foot on prison grounds, she was virtually diagnosis and medication-free, he says.
During her health screening at reception, Jennifer admitted to a suicide attempt in 2002. She was put on an “observation cell” order, the standard response to inmates deemed to be a risk to themselves or others.
“A really large proportion of girls told me I was absolutely stupid for admitting to – and officers told me I was stupid for admitting to – a self harm incident. Most of [the women] seem to have some kind of mental health issue but they didn’t tell the officers or the welfare or the nurses because of ... their treatment of [mentally ill] people. People are terrified of going into those safe cells and after having been in them, I’m terrified of going into them,” she says.
According to a Corrective Services NSW spokesperson, an observation cell is “designed to minimise the opportunities of self harm, so therefore it’s got no hanging points, they’ve got special blankets, it has camera observation and nothing sharp or unscrewable.”
She says the time an inmate is consigned to an observation cell “varies, but it’s usually a short time, like a day”.
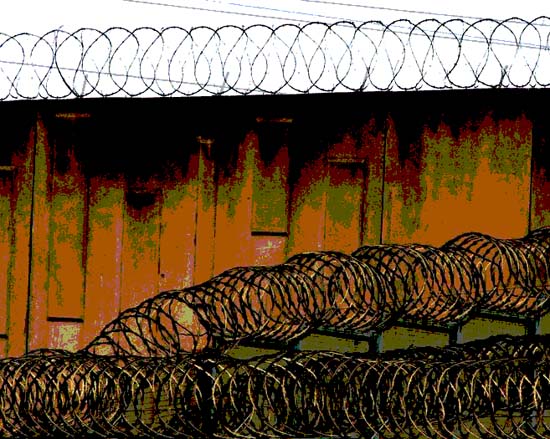
Security lockdown
Jennifer spent four days in an observation cell due to a two-day security lockdown in which inmates were forbidden from leaving their cells.
“It was horrific,” she says.
“The lights are kept on 24 hours a day and the officers are absolutely horrible to you while you’re in there. The air-conditioning is switched to freezing then switched off at four o’clock in the morning so you go to sleep in your tracksuit and wake up drenched in sweat thinking you’re sick.
“I was refused medical treatment while I was in there. I was refused access to a telephone. I wanted to call the Ombudsman. After I said I wanted to call the Ombudsman they specifically refused to let me out of the cell.”
She describes how confusion, anger and sleep deprivation gave way to hysteria and paranoia. By the fourth day, she says, she was lying on the floor “unable to eat, shaking constantly, crying almost continuously and unable to sleep.”
Catriona McComish, a former senior assistant commissioner at Corrective Services NSW, says observation cells illustrate precisely why the prison system is incapable of rehabilitating the mentally ill.
“If someone is regarded as significantly distressed and is either self harming or is psychotic or is assessed as at risk of suicide in a hospital setting or a clinical setting, then you ensure that they stay with people; they’re calmed ... with medication and talk and company and assistance and support.
“Whereas in prison the kind of assessment would err - because of the inquiries that have been and because of the fear of the ramifications of death in custody - on the side of just containing the risk, which means containing the person,” says McComish, who served for 13 years in a number of senior roles at Corrective Services including five years as Director of Psychological Services.
“It is certainly not good for the longer term outcome. If you put someone who’s got a mental illness, who is actually at risk of suicide ... in [an observation cell, it] is going to make them much, much worse,” she says.
“They’re a symbol of all that’s wrong, that people like that end up in prison.”
* * *
The number of women being jailed in NSW has risen more than 60 percent in the past decade, compared to a 25 percent increase in the rate of imprisonment of men.
Of the state’s 850 women inmates, around 86 per cent have at least one psychiatric disorder, according to data from Corrections Health (now Justice Health). The 2003 study of NSW prisoners found that women outnumber men across all categories of psychiatric disorder. Two-thirds of women compared to 50 percent of men have a substance use disorder; 60 percent (compared to 38 percent of men) have a mental disorder; 55 per cent (compared to 30 percent of men) have an anxiety disorder; and 29 per cent (compared to 18 per cent of men) have an affective disorder such as depression.
Such extraordinary levels of mental illness have significant consequences for the women’s prison environment, says McComish, who left the department in 2006.
“In corrections, just about everyone would say – whether it’s medical staff or program staff or correctional staff – that they much prefer to work in a male prison than a female prison. No one really wants to work with them,” she says.
“They often get angry and aggressive and demanding and needy and they cut themselves and it’s messy and they don’t get better, so staff become punitive.”
But the behaviour of custodial officers is only one dimension of a much larger structural problem. The lack of beds for women in minimum and medium security correctional facilities means hundreds of women are imprisoned in higher security facilities than actually required by their classification.
At the time of the 2009 NSW Inmate Census , 72 percent of the state’s 854 women prisoners had a minimum security classification yet only 32 per cent were actually imprisoned in minimum security centres. Conversely, only two women inmates had maximum security classifications yet 214 women were being held in maximum security centres across the state.
Strict conditions
Prisoners in maximum security must abide by strict conditions that limit personal property, visit entitlements and access to programs, regardless of their classification. They also cannot access study leave or work release.
Prison reformers argue that the classification system discriminates against the mentally ill, because it equates mental health needs – which can manifest as difficult or unco-operative behaviour – with heightened risk concerns. Studies show the mentally ill are also more likely to reoffend and re-enter prison under higher security classifications. As a result, the women who most urgently need skills, education and support are least able to access work release, study leave and programmes.
“So in the women’s system you also end up with an extraordinary mixture in terms of needs – so you have women who are psychotic, women who have a significant intellectual disability, women who have severe behaviour problems,” McComish says.
“And because units are small, they all end up together and the unit becomes dysfunctional ... [It] essentially becomes a punitive place were there needs to be significantly high levels of security and lockdown because the mix is so volatile.”
* * *
“I grew up in a very abusive household – physical and emotional abuse on a daily basis. I ran away from home when I was 16 to get away from my mother. My father died of alcoholism when I was five years old. I found his body in the kitchen,” Jennifer says.
“Through my late teens and early 20s I was a heroin addict and sex worker and homeless and all of those things that you are when you live that way.”
Then in February this year, she was hit by a motorbike when she was crossing the road. The police officer who came to take her statement informed her there was an outstanding warrant for her arrest over a property crime committed more than a decade ago, when she was drug-addicted and living on the streets.
Life stories of violence and disadvantage, where the line between victim and offender is blurred and broken, are common among women prisoners. Up to 85 per cent of women inmates are survivors of sexual abuse or incest; 70 percent are victims of physical violence; 66 percent have a drug or alcohol addiction; 40 percent have attempted suicide; and 30 percent were removed from their families as children.
Poverty, homelessness and welfare dependence bring women into greater contact with authorities, however the characteristics of women offenders suggest that women actually pose little threat to the community. At the time of the 2009 NSW Inmate Census, "homicide and related offences" were the most serious offence for only 7.6 percent of women inmates; most were imprisoned for non-violent offences related to poverty and drug dependence.
Because the nature of women’s imprisonment reflects women’s position in society, they often suffer disproportionately in prison. Kat Armstrong, spokesperson for the Women in Prison Advocacy Network NSW and a former inmate, points out that a large proportion of women entering prison are single parents or primary caregivers, if not for their own children then for their partner’s.
“The frustration and the sheer anguish of being separated from your children, not knowing where your children are, who’s looking after them – women have severe disturbances as a result of that,” Armstrong says.
Even women who do have partners are often not financially or emotionally supported during their incarceration. This is in contrast to many male prisoners whose partners on the outside continue to take care of their family and property while they are in jail. Partners also contribute to inmates’ jail accounts and send clothing and other personal items, Ms Armstrong says.
“You go to a men’s visiting section and it’s full of women and children. You go to a women’s visiting section and you could count on one hand how many men are there, as in partners.” Armstrong says.
“[The partners] either leave or [are] in jail as well or they come for the beginning and then can’t deal with it and don’t come anymore.”
Wages system unfair
Inmates who do not receive help from the outside must support themselves entirely on prison wages. With the money they earn (prisoners are paid between 60 cents and $1.50 per hour, depending on the type of work), they must buy their own toiletries, underwear and clothing when prison-issued clothing needs replacing, and other items like cigarettes.
Women prisoners are also disadvantaged by a wage system that values the labour of prisoners over their education.
“The majority of women need the money so they’ll try to work rather than do programmes or education, [which is] one of the lowest paying wages ... [at] $22 a week.”
In the end, Armstrong says, most women leave prison as unskilled and uneducated as when they entered. Faced with rebuilding their lives in a society that heavily stigmatises women ex-prisoners, it is little surprise that many find the obstacles insurmountable.
Jennifer is one of a minority of women who had a family and a home to return to upon her release. Nevertheless, she says, the damage to her life and health has been significant.
“I’ve pretty much lost my entire social circle ... I’ve lost a tremendous amount of respect from people that I used to know. I’ve lost a tremendous amount of respect from my son; it’s made parenting him quite difficult.”
This is a system that sets women up to fail, prison reformers argue, and the statistics seem to agree. According to the 2010 report of the Auditor-General , about 43 percent of NSW offenders return to prison within two years. Other statistics, which take into account reoffenders who receive non-custodial sentences place the rate of recidivism closer to 68 percent.
* * *
With the closure of psychiatric institutions and the failure of governments to divert savings into community-based support services, the reality is that for a tiny minority, prison has become the best and sometimes the only option.
Renee* was 14 when she was first admitted to a psychiatric hospital. Now in her thirties, she has lived in 10 psychiatric hospitals and served two jail sentences. She was re-arrested earlier this year after setting fire to her mattress at the psychiatric hospital where she lived. She is now at Silverwater Women’s Correctional Centre, awaiting sentencing.
“She keeps doing all this stuff to go back to jail ... she stopped taking her medications, smashed the TV,” says her sister, Lynette. “I spoke to her today and she said to me there’s a part of her that keeps wanting to go back to jail ... It’s like jail became safe.”
Renee is diagnosed with paranoid schizophrenia, epilepsy and personality disorder. She also has a history of substance abuse. She was first incarcerated in 2008 on assault charges, after throwing coffee on a nurse at the psychiatric hospital where she lived. She spent 11 weeks in Silverwater Women’s Correctional Centre.
Prison rape
Less than six months after her release, she was jailed again on a second assault charge. Only after she was released for the second time did Renee confide to her sister that she had been held down and raped by three women inmates in the prison’s mental health unit.
“She didn’t tell the [prison] staff ... she was too scared to tell anyone in authority,” Lynette says.
Renee is now back in the unit where she says she was raped. Lynette shakes her head in disbelief.
“I [find] it very hard to understand how you could feel safe in that environment and want to go back into it,” she says.
“But one thing ... she said [was that] some of the prison officers treated her better than some of the mental health workers ... and I’m wondering if that’s why she wants to go back to jail – because she gets treated better there than in the mental health system.”
Eileen Baldry, an associate professor at the University of NSW and a long-standing critic of the prison system, says this may well be the case.
“I have heard from many parents and families of prisoners who have mental illness ... that this is one of the only times that their [family member] ... has actually received ongoing mental health care and has become sane,” Dr Baldry says.
“In my view [this] says more about the terrible state of healthcare for poor and disadvantaged people in our community ... People shouldn’t have to go to prison to get ... mental health care.”
Yet prisons have become the de facto therapeutic dumping place for huge numbers of people with serious and complex health issues – which is not the fault of prisons, but of governments and the community, Dr Baldry says.
“I think the bigger picture is that we as a society and a community have to think differently ... [We] have to understand that it’s no light thing to send somebody to prison,” she says.
“Sending someone like that to prison doesn’t deter them the next time. It doesn’t teach them a lesson because often when they commit a crime they’re under the influence of drugs or they are having a psychotic episode or their intellectual capacity is fairly low and it doesn’t compute for them.”
In the meantime women like Renee, deemed too hard to handle, continue to be passed from one institution to the next, into jail and back again.
“The local mental health services can’t cater to them. I’ve tried to get help in the middle of the night for my sister and ... they tell you to call the police and you don’t want to call the police because you know what the outcome will be,” Lynette says.
“My sister is really hard to handle but there’s a really beautiful side to her ... She may never lead the ... life that you and I lead but if there could be some normal life for her ,” Lynette says. “They’re either in [psychiatric hospitals] or they’re in jail ... Society can’t cope with them and sometimes they are dangerous to other people, but why should jail be the answer?”
*Name changed
Inga Ting is a journalist who works with the Australian Centre for Independent Journalism. This article was first published in Crikey.